January marks Cervical Health Awareness Month. Around 11,500 Americans are diagnosed with cervical cancer each year, according to data from the Centers for Disease Control and Prevention, and in 2022, over 4,000 people died from the disease despite it being considered highly preventable.
White women are more likely to be diagnosed with cervical cancer than any other group, CDC data shows. However, a 2022 study published in the Journal of Clinical Oncology found greater rates of diagnosis were mostly due to higher levels of screening. Black women have the lowest screening rates, the study found, "strongly driven by insurance and site of care, underscoring the value of addressing systemic inequity."
For decades, a Pap smear has been the standard way to detect cervical cancer. The uncomfortable and, for some, painful procedure entails using a small brush or spatula to lightly scrape the cervix to gather cells. Cells are then examined under a microscope for precancers or other abnormalities. This procedure also tests for the human papillomavirus, which can cause cell changes on the cervix that lead to cancer if not treated early.
But soon, a self-swab approved in May 2024 by the Food and Drug Administration might help people avoid the invasive procedure—and save lives. Patients will be able to use an at-home kit to swab their vaginal walls and send it to a lab to be tested for HPV. It's part of the National Cancer Institute's Cervical Cancer 'Last Mile' Initiative, which will study the accuracy and effectiveness of self-testing at 25 clinical sites nationwide. Participant enrollment began this past summer.
"Self-collection can expand access to screening and reduce barriers, which will give more people the opportunity to detect, treat, and ultimately survive cancer," Karen E. Knudsen, CEO of the American Cancer Society, said in a press statement after the announcement.
Northwell Health partnered with Stacker to explore disparities in cervical cancer deaths and what a new testing mechanism could mean for prevention. Data is from the Centers for Disease Control and Prevention.
Editor's note: Pap smears are a cervical cancer screening tool and are recommended for people with cervixes, not all of whom identify as women. In this article, we have used gender-neutral terms when possible. We use gendered language in the characterization of data to stay true to how sources collected and presented the information.
Photo illustration by Elizabeth Ciano // Shutterstock
An opportunity to improve screening rates
Early detection is the key to preventing cervical cancer deaths. Yet, data spanning June 2016 to May 2019 published in the American Journal of Preventive Medicine in October 2023 suggests that only two-thirds of at-risk people are up-to-date on screenings. For Black people, that number drops to about half.
One factor that impacts screening rates includes whether people have insurance coverage. A 2022 KFF Women's Health Survey found that 42% of uninsured women had received a cervical cancer screening in the past year, compared to 64% with private insurance and 56% of those with Medicaid. However, even when screening rates are equal, disparities in care and delays in treatment have contributed to lower survival rates among those who are diagnosed with cancer.
Within the health care system, racial bias and discrimination contribute to disparities in mortality rates. Differences in the quality of screening techniques and a lack of representation of people of color in the development of screening guidelines and clinical trials are just a few forms of systemic bias.
Research from the American Cancer Society released in January 2020 showed that even when adjusting for age, sex, and stage of diagnosis, Black people are 33% more likely to die from cancer than white patients. For American Indians and Alaska Natives, the risk of dying from cancer is 51% higher.
Where a patient lives can also affect screening rates. In 2022, less than half of rural residents received a Pap smear in the prior year, compared to about 2 in 3 urban residents, according to another study published in the Journal of the American Medical Association, which looked at data from 2019 to 2022.
The hope is that self-collection will improve screening rates among underserved populations in the U.S. Similar strategies have been adopted in Denmark, Sweden, and the Netherlands to much success. In Australia, more than 315,000 people have opted to self-collect since an initiative was launched in 2022. By March 2024, more than 1 in 4 screenings were done using collection kits in Australia.
Northwell Health
Racial disparities require more than one solution
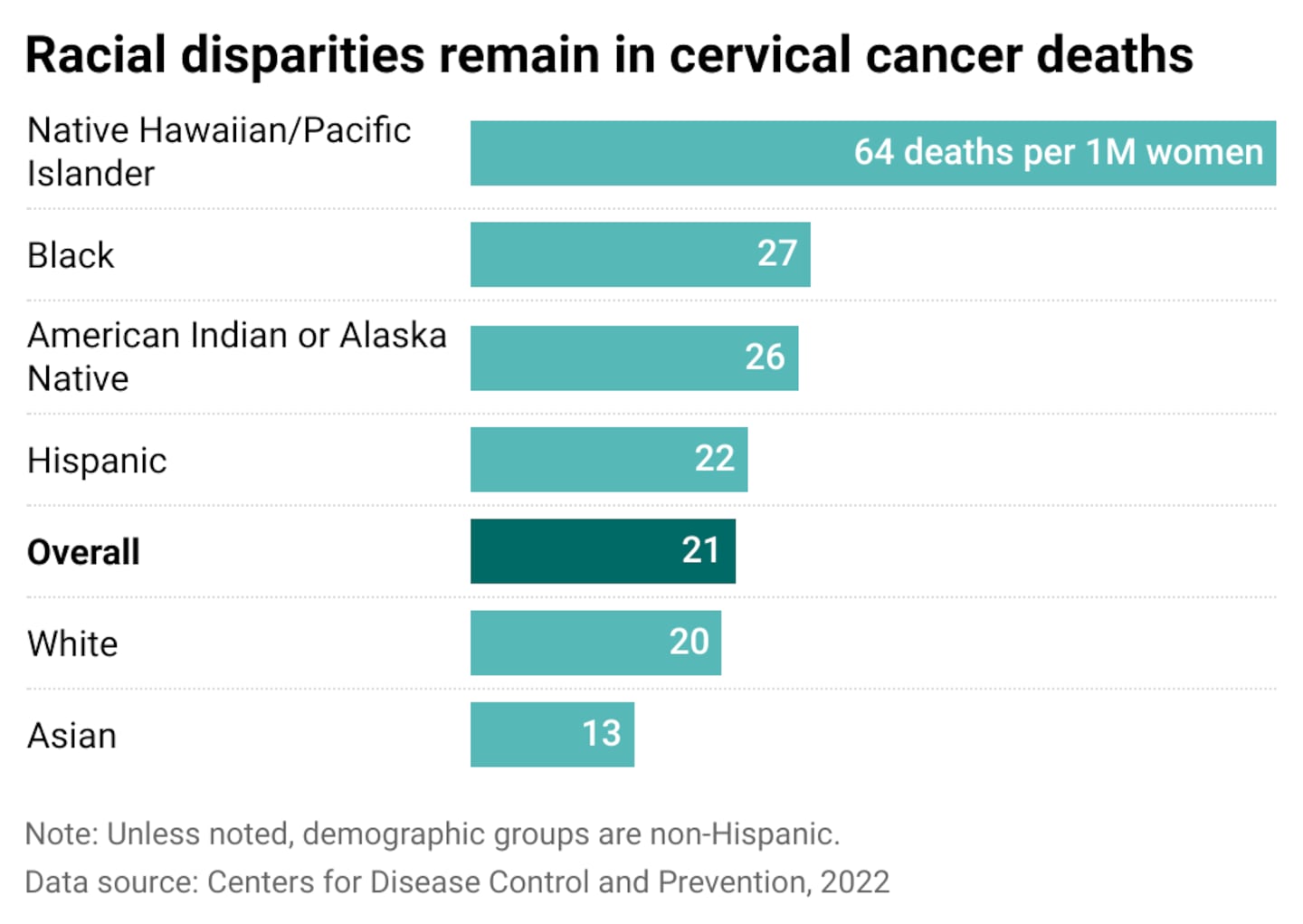
In 2022, there were about 21 cervical cancer deaths for every million women living in the United States, according to the CDC. Broken down by race, Native Hawaiians and Pacific Islanders have the highest rates of cervical cancer deaths in the U.S.
Again, lack of access to quality care plays a role. Because Native Hawaiian and Pacific Islanders get tested less frequently, they are more likely to receive a late-stage cancer diagnosis, according to American Cancer Society research. This is particularly true among Native Hawaiians. While screening rates are generally similar across the state of Hawai'i, in 2022, just 79% of Native Hawaiian women between 25 and 65 years old were up-to-date on cervical cancer screenings, compared to 88% of white women.
The problem is most acute in the six U.S. territories in the Pacific Islands, which includes Guam, American Samoa, and the Federated States of Micronesia, according to data analysis on more than 400 cervical cancer cases published in 2024 in JAMA Oncology. Researchers found nearly 7 in 10 cervical cancer cases were diagnosed at a late stage from 2007 to 2020.
Black and Indigenous women also have elevated death rates from cervical cancer due to a lack of follow-up care after an abnormal screening. While insurance coverage and socioeconomic factors are at play, medical distrust also plays a role. This is particularly true in the field of gynecology, which the medical community built on the backs of enslaved people in the Antebellum South.
J. Marion Sims is widely credited with developing many of the modern-day tools still used in gynecology today, including the speculum, a hinged tool inserted into the vagina and expanded to get a better view of the cervix. The first version was made of bent metal spoons, which Sims used while examining enslaved people in Montgomery, Alabama.
In recent years, many have reevaluated Sims' legacy in the field, largely due to the inhumane treatment of his Black patients, whom he rarely gave anesthesia during painful procedures. His studies reinforced the false belief that Black patients have higher pain thresholds, leading to pain being dismissed and downplayed even today.
This history is a testament to the importance of culturally competent care, the ability to communicate and collaborate with people from different backgrounds and understand how their identity and culture play a role in their views and understanding of health care A case study of 40 Black and Hispanic women in Texas found when provided with culturally competent education and a self-sampling kit for HPV, screening rose from about 6 in 10 to 9 in 10 among both groups.
Northwell Health
Improving preventative care across the country
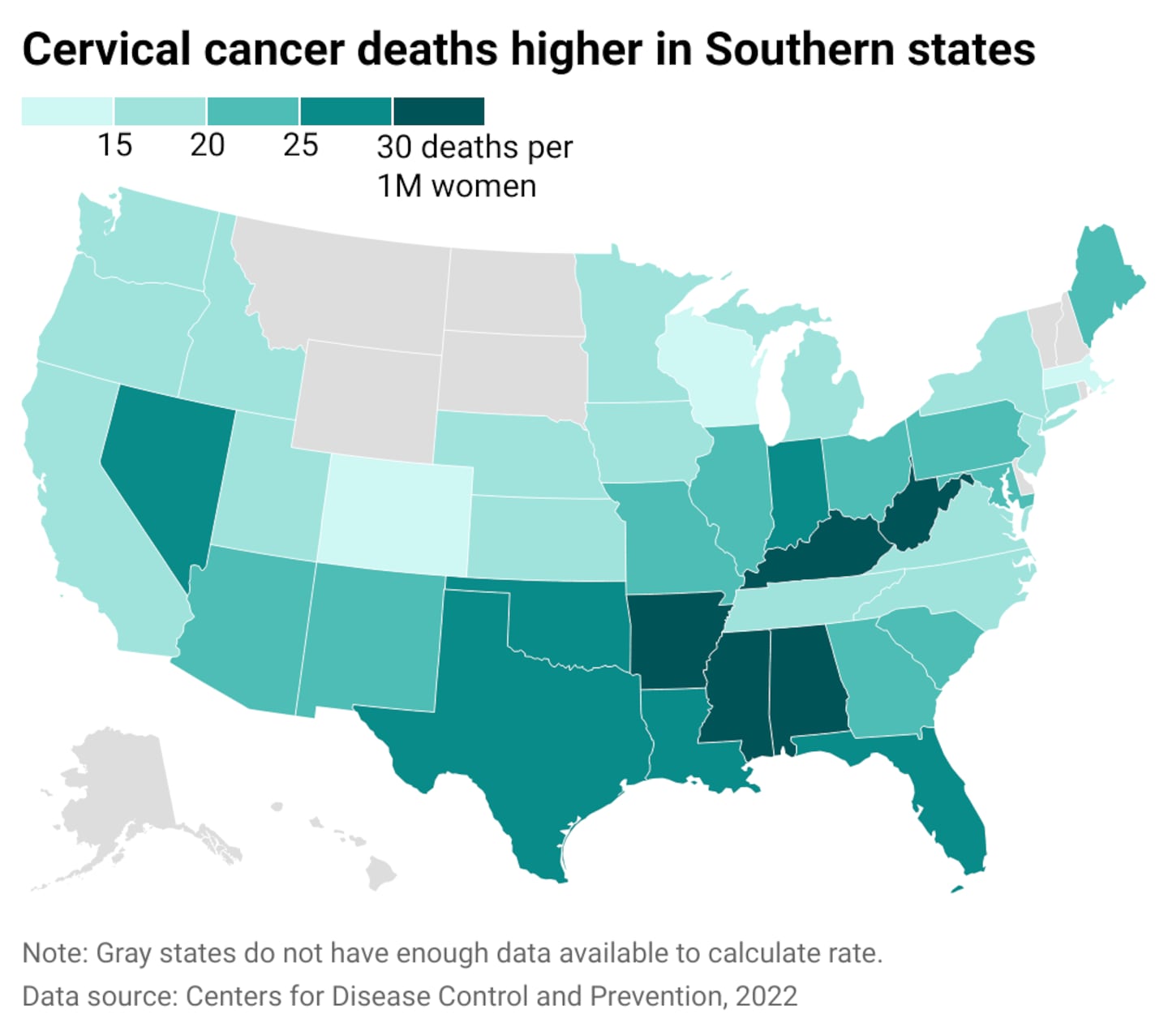
In the Lower 48, cervical cancer deaths are higher in states with large uninsured populations and a high percentage of Black residents.
In Mississippi, which has the highest poverty rate in the nation, there are about 4 cervical cancer deaths per 100,000 women. The state health department's Breast and Cervical Cancer Program provides free Pap screenings at some clinics for uninsured people between the ages of 40 and 64. Kentucky, which has the third-highest cervical cancer rate in the country, runs a similar program for those 21 and older who do not have insurance and whose household income is less than 250% of the federal poverty level. Over 16% of the state's population lives below the poverty line.
However, while self-screening will undoubtedly increase early detection, it is just one factor in curbing cervical cancer deaths. Other preventative measures need improvement, including HPV vaccination rates, which have proven to be one of the most effective tools in reducing cervical cancer.
Globally, cervical cancer rates are higher in low- and middle-income countries. In 2020, the World Health Organization launched the Cervical Cancer Elimination Initiative, which includes the goal of vaccinating 90% of girls worldwide for HPV by the age of 15.
Self-exams don't replace pelvic exams, and encouraging follow-up appointments after an abnormal test is also important. A study of more than 160,000 women in New Mexico published in Preventative Medicine found that between January 2015 and August 2019, only half who tested positive for cancer-causing HPV cells followed guidelines and received a biopsy within six months. Three in 10 had not followed up within 18 months.
While it's clear continuous care and monitoring are necessary to prevent cervical cancer deaths, a holistic approach valuing the importance of self-care in cancer prevention is also vital.
Story editing by Alizah Salario. Additional editing by Kelly Glass. Copy editing by Kristen Wegrzyn.
This story originally appeared on Northwell Health and was produced and distributed in partnership with Stacker Studio.